Most of us are well aware of the importance of wearing sunscreen when we venture outdoors to protect our skin from the harsh rays of the sun. However, what many people may not realise is that wearing sunscreen indoors is just as crucial, especially in regions like Australia where the summer sun can be particularly relentless.
The scorching Australian sun is notorious for its intensity, and its harmful ultraviolet (UV) rays can penetrate through windows, glass, and even clouds, reaching us indoors. This means that even when we’re inside our homes or offices, our skin is still vulnerable to UV damage. Additionally, exposure to artificial sources of light such as fluorescent bulbs and electronic screens can also emit low levels of UV radiation, further contributing to the cumulative UV exposure our skin experiences.
Here are some compelling reasons to consider wearing sunscreen indoors:
Protection Against UV Exposure & Skin Cancer
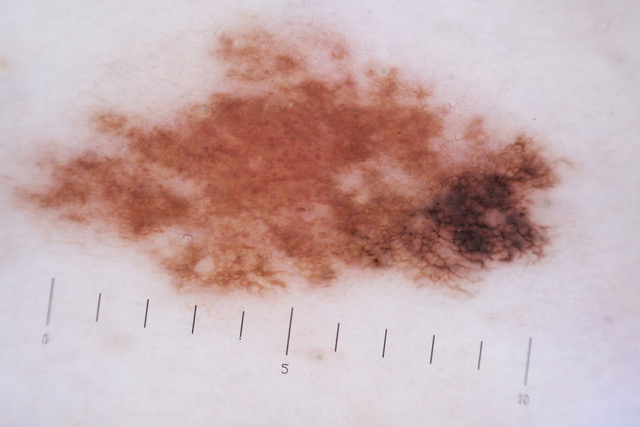
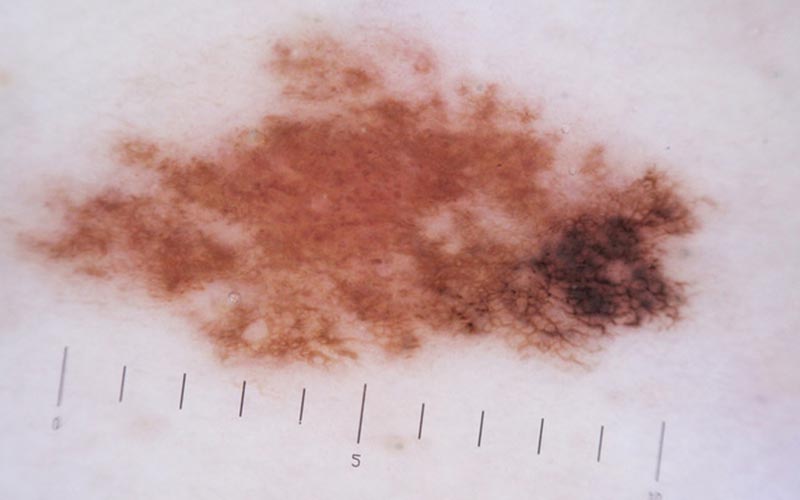
Sun’s ultraviolet (UV) rays are particularly intense, protecting your skin against UV exposure is paramount to prevent skin cancer, including melanoma, one of the deadliest forms of cancer. UV radiation is a known carcinogen, and prolonged exposure to UV rays significantly increases the risk of developing skin cancer. By wearing sunscreen indoors, you can mitigate this risk and safeguard your skin’s health.
Sunscreen serves as a vital defence against the harmful effects of UV radiation. It creates a protective barrier on the skin’s surface, absorbing and deflecting UV rays before they can penetrate the skin. By applying sunscreen regularly, even when indoors, you can reduce your risk of sunburn, premature ageing, and skin cancer caused by UV exposure.

Melanoma, in particular, poses a significant health threat in Australia due to the country’s high levels of UV radiation. Melanoma develops in the melanocytes, the pigment-producing cells in the skin, and can metastasise rapidly if not detected and treated early. UV exposure is a major risk factor for melanoma, making sun protection measures, including wearing sunscreen indoors, essential for preventing this deadly disease.
Moreover, UV radiation not only damages the skin’s DNA, leading to mutations that can trigger cancerous growth but also suppresses the immune system’s ability to detect and destroy abnormal cells. This dual mechanism of UV-induced damage and immunosuppression underscores the importance of consistent sun protection practices, including sunscreen use, to reduce the risk of skin cancer.
Prevention of Photoaging
Protecting your skin against UV radiation is essential not only for preventing skin cancer but also for minimising the visible signs of ageing, a process known as photoaging. UV rays can penetrate deeply into the skin, even passing through window glass and clouds, making sun protection necessary both indoors and outdoors, especially in Australia where UV radiation levels are high.
Photoaging occurs as a result of prolonged exposure to UV radiation, leading to the breakdown of collagen and elastin fibers in the skin. Collagen and elastin are proteins responsible for maintaining the skin’s firmness, elasticity, and overall youthful appearance. When these fibers are damaged by UV rays, the skin loses its ability to bounce back, resulting in wrinkles, fine lines, sagging, and uneven pigmentation.
Regular exposure to higher levels of UV radiation, common in Australia due to its geographical location and climate, accelerates the photoaging process. Even brief exposure to UV rays indoors, such as when sitting near a window or under fluorescent lights, can contribute to cumulative UV damage over time.

By wearing sunscreen indoors, you can help prevent photoaging and maintain healthier, more youthful-looking skin. Sunscreen forms a protective barrier on the skin’s surface, blocking harmful UV rays and reducing their ability to penetrate and damage the skin. Additionally, sunscreen helps to neutralise free radicals generated by UV exposure, which can further contribute to skin aging.
Incorporating sunscreen into your daily skincare routine, regardless of whether you’re indoors or outdoors, is crucial for preserving your skin’s youthful appearance and minimising the visible signs of ageing. Remember, prevention is key when it comes to photoaging, and wearing sunscreen consistently is one of the most effective ways to protect your skin from UV-induced damage and maintain a more youthful complexion.
Skin care routine to protect your skin indoors
Maintaining a diligent skincare routine is essential for protecting your skin indoors, especially in a country like Australia with its harsh sun exposure. Here are some key steps to incorporate into your indoor skincare regimen:
- Keep your skin moisturised: Indoor environments, particularly those with air conditioning or heating systems, can strip moisture from your skin, leading to dryness and irritation. Use a hydrating moisturiser regularly to replenish lost moisture and keep your skin soft and supple. Look for products containing ingredients like hyaluronic acid, glycerin, and ceramides, which help to attract and retain moisture in the skin.
- Apply sunscreen as needed: While it’s tempting to think that you’re safe from UV rays indoors, the reality is that harmful UVA rays can penetrate through windows, putting your skin at risk of damage. To safeguard against UV exposure, apply a broad-spectrum sunscreen with at least SPF 30 to all exposed areas of skin, including your face, neck, and hands. Reapply sunscreen every two hours, especially if you’re near windows or spending extended periods of time outdoors.
- Do not expose your skin without protection: Even if you’re spending the majority of your time indoors, it’s important to avoid exposing your skin to harmful UV radiation without protection. Keep curtains or blinds closed during peak sun hours to minimise UV exposure indoors. Additionally, consider wearing protective clothing, such as long-sleeved shirts, pants, and wide-brimmed hats, to shield your skin from direct sunlight.